Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Google Podcasts | Spotify | Email | RSS | More
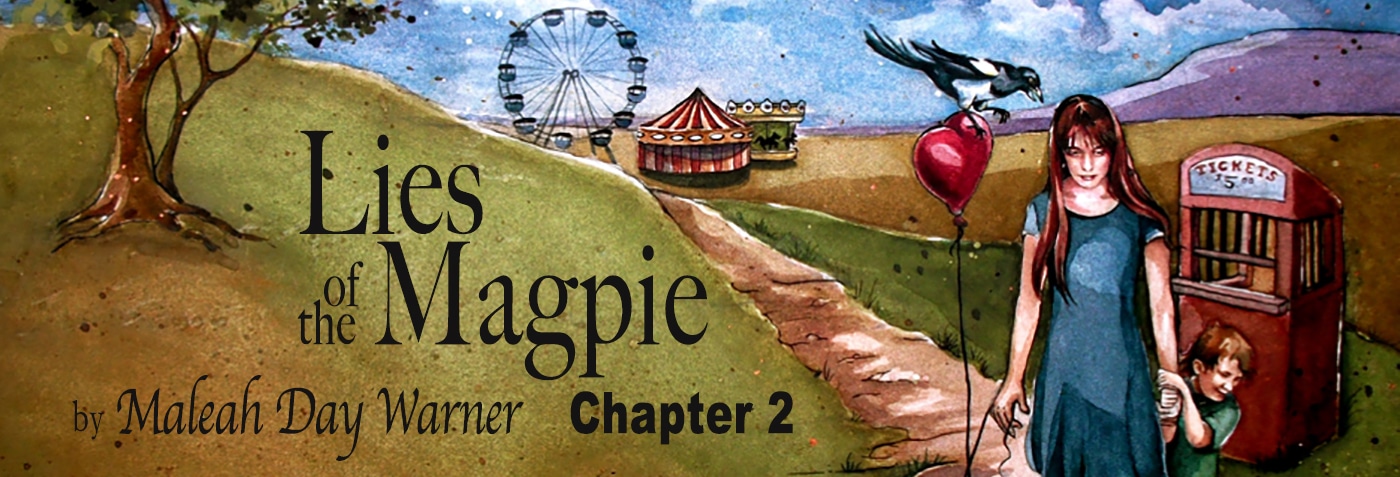
Ch. 2 Lies of the Magpie
The story of my journey healing through postpartum depression and chronic illness.
The thing Aaron remembers most about me from college is my fast-paced walk around campus. His tennis class met at three o’clock at the courts across from my off-campus housing. For weeks he watched me leave my apartment, hurry across the road, rush past the tennis courts, short cut across the grass and disappear into the Humanities Building. His tennis partner noticed him staring and said, “Don’t waste your time. That is Maleah Day. She is the Academic Vice President. Ten bucks says you can’t get her to stop to talk to you. She walks that fast everywhere she goes.”
It was my sophomore year. I was ten years older than the straggly nine-year-old girl from Ms. Wickersham’s fourth grade class. My bean-pole figure had filled out in a few key places. Two years of orthodontic work and contact lenses had tamed my profile, but my ambition—if possible—was still as potent. I’d traded my dream of becoming a firefighter and astronaut to becoming an Airforce pilot and a foreign ambassador. I declared a Political Science major and carried an application for the Peace Corps in my backpack.
Still, I’d never forgotten my dream to become Mrs. Murry from A Wrinkle in Time and have my own kitchen/chemistry lab. My scholarship covered full tuition and fees, regardless of number of credit hours, so in addition to my social science courses, I registered for a Biochemistry Series, Anatomy, Microbiology, and Physiology. These would cover all lab science prerequisites, just in case I changed my mind about Foreign Diplomacy and decided to apply to Medical School. It was a good plan, I thought, to keep both options open.
Play button above to hear the full chapter.
Listen to Chapter 1: https://maleahwarner.com/?p=1258&preview=true&_thumbnail_id=1269
Listen to the Introduction of Lies of the Magpie https://maleahwarner.com/new-summer-series/
Book Cover Art by:
Bethany Baker of Midsummer Studios https://midsummerstudios.weebly.com/